Periodontal Disease – The Mouth Body Connection
Click each link below for more information
Understanding inflammatory load
This is a newer concept in medicine that is affecting the way we look at many of the diseases that affect the human body. Years ago, the term bacterial load was used to explain how a disease started and progressed. Simply explained, the absolute numbers of disease-producing bacteria predicted the initiation and progression of a disease. What many researchers noted was some patients had a low concentration of pathogenic bacteria and severe disease. The opposite was also true; high concentration of bacteria with minimal or no disease. What was discovered was that there was a tremendous degree of variability from patient to patient in how they responded to these bacteria. What they found was that some patients are hyper-responders. A low number of bacteria produce a tremendous amount of inflammatory mediators. These mediators can cause disease or ramp up existing disease. The inflammatory mediators remain the same whether they are produced by periodontal disease or a skinned knee. Periodontal disease, however, constantly causes the mediators to be churned out into the bloodstream. These mediators then travel to distant sites in the body where they can cause existing disease to increase in severity or in some cases to start the disease process.
Periodontal disease, systemic Inflammation and the risk of cardiovascular disease (CVD).
Periodontal Disease and Alzheimer’s Disease
Researchers have found inflammatory load will have a direct affect on the onset and progression of Alzheimer’s disease. A 2015 paper by Kamer showed a positive association between periodontal disease and Alzheimer’s progression rate. They hypothesized that inflammatory mediators produced by periodontal disease would travel via the blood stream to the brain and up-regulate an inflammatory response in brain tissue.
Study: Kramer 2015 –
Periodontal disease associates with higher brain amyloid in normal elderly
https://www.ncbi.nlm.nih.gov/pubmed/25491073
__________________________________________
Study: January 2019 –
Periodontal disease bacteria linked Alzheimer’s Disease.
A recent study has periodontists, experts in the treatment, diagnosis, and prevention of periodontal disease, encouraging patients to maintain gum health in an effort to reduce their Alzheimer’s disease risk.
The study, published in the journal Science Advances, uncovered a potential link between P. gingivalis, the bacteria associated with periodontal disease (commonly known as gum disease) and Alzheimer’s. Researchers analyzed brain tissue, spinal fluid, and saliva from Alzheimer’s patients—both living and deceased—and found evidence of P. gingivalis. Gingipains, the toxic enzyme secreted by P. gingivalis, were found in 96 percent of the 53 brain tissue samples examined, with higher levels detected in those with the pathology and symptoms of Alzheimer’s disease.
Additionally, researchers including co-author Mark I. Ryder DMD, Professor of Periodontology at the University of California, San Francisco, noted that the presence of P. gingivalis increased the production of amyloid beta, a component of the amyloid plaques whose accumulation contributes to Alzheimer’s. The study confirmed via animal testing that P. gingivalis can travel from the mouth to the brain and that the related gingipains can destroy brain neurons. These findings are noteworthy in that they suggest a biological mechanism for how periodontal disease bacteria may play a role in the development and progression of Alzheimer’s.
https://www.perio.org/consumer/alzheimers-and-periodontal-disease
____________________________________________
Study: January 2019 –
Porphyromonas gingivalis in Alzheimer’s disease brains
Periodontal Disease and Alzheimer’s Disease
Researchers have found inflammatory load will have a direct affect on the onset and progression of Alzheimer’s disease. A 2015 paper by Kamer showed a positive association between periodontal disease and Alzheimer’s progression rate. They hypothesized that inflammatory mediators produced by periodontal disease would travel via the blood stream to the brain and up-regulate an inflammatory response in brain tissue.
Study: Kramer 2015 –
Periodontal disease associates with higher brain amyloid in normal elderly
https://www.ncbi.nlm.nih.gov/pubmed/25491073
__________________________________________
Study: January 2019 –
Periodontal disease bacteria linked Alzheimer’s Disease.
A recent study has periodontists, experts in the treatment, diagnosis, and prevention of periodontal disease, encouraging patients to maintain gum health in an effort to reduce their Alzheimer’s disease risk.
The study, published in the journal Science Advances, uncovered a potential link between P. gingivalis, the bacteria associated with periodontal disease (commonly known as gum disease) and Alzheimer’s. Researchers analyzed brain tissue, spinal fluid, and saliva from Alzheimer’s patients—both living and deceased—and found evidence of P. gingivalis. Gingipains, the toxic enzyme secreted by P. gingivalis, were found in 96 percent of the 53 brain tissue samples examined, with higher levels detected in those with the pathology and symptoms of Alzheimer’s disease.
Additionally, researchers including co-author Mark I. Ryder DMD, Professor of Periodontology at the University of California, San Francisco, noted that the presence of P. gingivalis increased the production of amyloid beta, a component of the amyloid plaques whose accumulation contributes to Alzheimer’s. The study confirmed via animal testing that P. gingivalis can travel from the mouth to the brain and that the related gingipains can destroy brain neurons. These findings are noteworthy in that they suggest a biological mechanism for how periodontal disease bacteria may play a role in the development and progression of Alzheimer’s.
https://www.perio.org/consumer/alzheimers-and-periodontal-disease
____________________________________________
Study: January 2019 –
Porphyromonas gingivalis in Alzheimer’s disease brains
Periodontal Disease and Diabetes
The association between diabetes and periodontal disease has been studied for more than 50 years. Study after study has shown a direct relationship in the severity of diabetes to periodontal disease. What is interesting about this relationship is that it is a positive feedback loop. Diabetes makes periodontal disease worse which in turn feeds back and makes diabetes worse.

Periodontal Disease and Cardiovascular Disease and Stroke
Physicians are now accepting that periodontal inflammation is an important factor in heart disease and stoke. An article by Souvik Sen M.D. looked at 6,736 subjects over 15 years. Patients with periodontal disease had a 2.1 times higher risk of stroke. What is very interesting is that, statistically, the increased risk conferred by periodontal disease was similar to the risk conferred by high blood pressure.
Study: Periodontal Disease, Regular Dental Care Use, and Incident Ischemic Stroke
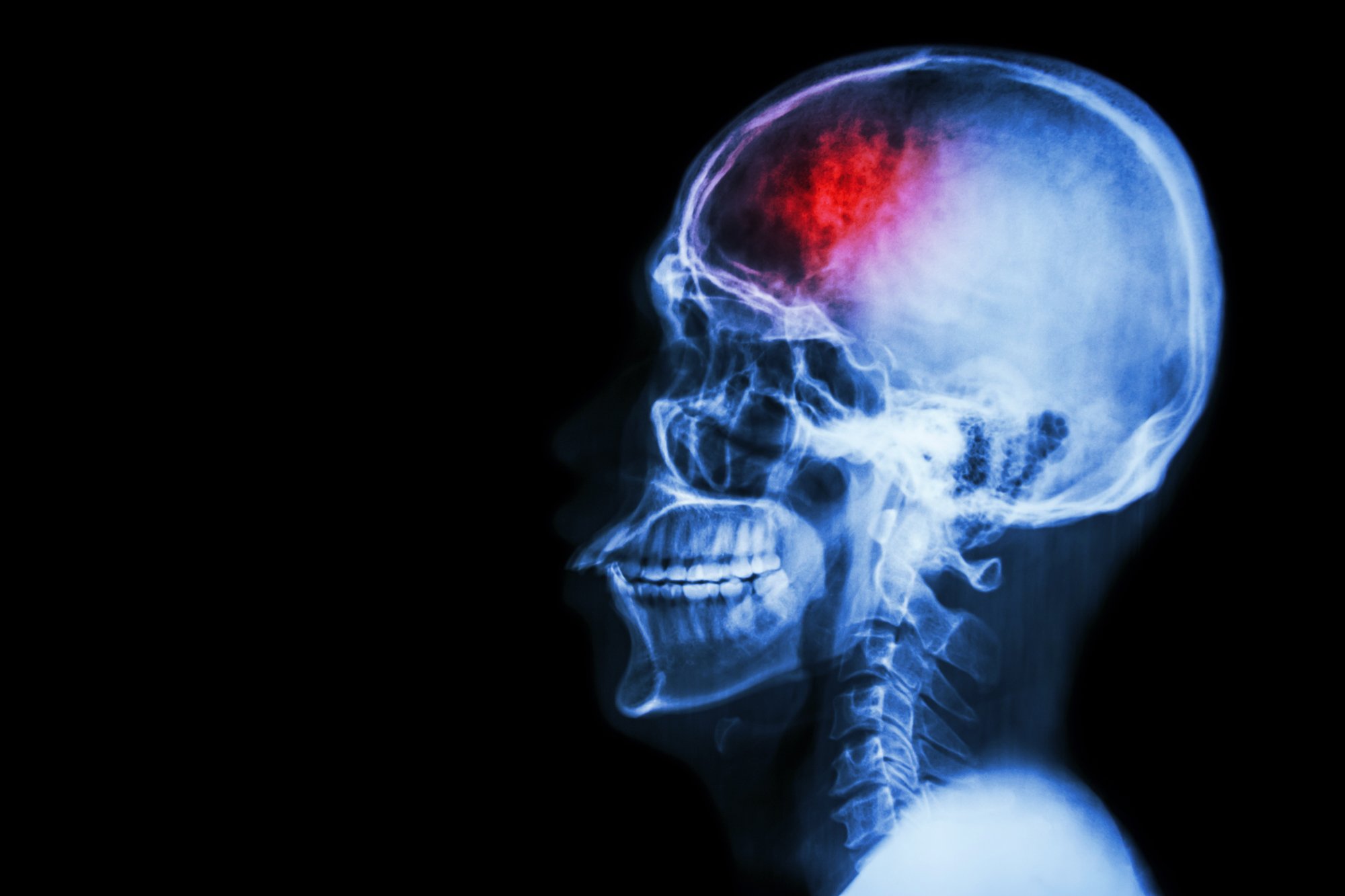
Periodontal Disease and Cardiovascular Disease and Stroke
Physicians are now accepting that periodontal inflammation is an important factor in heart disease and stoke. An article by Souvik Sen M.D. looked at 6,736 subjects over 15 years. Patients with periodontal disease had a 2.1 times higher risk of stroke. What is very interesting is that, statistically, the increased risk conferred by periodontal disease was similar to the risk conferred by high blood pressure.
Study: Periodontal Disease, Regular Dental Care Use, and Incident Ischemic Stroke
Periodontal Disease and Kidney Disease
Patients with kidney disease and periodontal disease have a significant increase in death over patients with healthy gums. Patients with kidney disease after 10 years had a death rate of 32% with healthy gums and 41% with periodontitis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5683458/
Both periodontal disease and chronic kidney disease are considered inflammatory conditions, and previous research has suggested that inflammation may be the common link between these diseases. Since untreated periodontal disease can ultimately lead to tooth loss, edentulous patients may have been exposed to chronic oral inflammation.
Periodontal Disease and Respiratory Disease
Periodontal disease inflammatory mediators that cause destruction of connective tissue in the mouth can also cause destruction of connective tissue in the lungs. This had been associated with a link between periodontal disease and chronic obstructive pulmonary disease, the 4th leading cause of death in the United States. This is especially important in patients living in long-term care facilities.
Study: Inpatients days in patients with respiratory diseases and periodontal disease
https://www.ncbi.nlm.nih.gov/pubmed/28128803


Periodontal Disease and Respiratory Disease
Periodontal disease inflammatory mediators that cause destruction of connective tissue in the mouth can also cause destruction of connective tissue in the lungs. This had been associated with a link between periodontal disease and chronic obstructive pulmonary disease, the 4th leading cause of death in the United States. This is especially important in patients living in long-term care facilities.
Study: Inpatients days in patients with respiratory diseases and periodontal disease
https://www.ncbi.nlm.nih.gov/pubmed/28128803
Periodontal Disease and Pregnancy
An increasing number of studies are confirming an association between periodontal disease and adverse outcomes in pregnancy. Periodontal disease places pregnant women at greater risk for preterm birth than alcohol consumption or smoking. A well-researched study by Offenbacher and colleagues found that women with severe periodontal disease were 7.5 times more likely to go into labor prematurely.
2006 Study: Periodontal Disease and adverse pregnancy outcomes:
A Systematic Review
https://www.ncbi.nlm.nih.gov/pubmed/16411989
